A common refrain in science fiction movies is the cautionary statement, “Just because we can doesn’t mean we should.” As new technologies such as CRISPR/Cas9 have made gene editing at precise locations in DNA possible, that sentiment has plagued ethicists and scientists alike regarding heritable human genomes.
The need for guidelines became apparent when Dr. Jiankui He, a researcher who worked in a lab in Shenzhen, China, announced the birth of two genome-edited infants in 2018. Dr. He used the CRISPR/Cas9 on the twin embryos to disable the gene that encodes a protein whose expression allows HIV to enter a cell — the implications of which may not be known for years or generations to come. In the aftermath of Dr. He’s announcement, the International Commission on the Clinical Use of Human Germline Genome Editing was established. The Commission, made up of experts in genetics and gene editing from around the world, recently published 11 guidelines citing scientific criteria for responsible clinical use of heritable human genome editing.
From the start, the Commission stated that heritable genome editing is not ready to be tried safely and effectively in humans, any initial clinical use should be limited to serious single-gene diseases, and only when it is permissible according to local regulations. Given the lack of evidence of potential long-term impact of editing heritable genes, members of the scientific community wonder if even laying out these strict parameters is wise.
The Promise of the Technology and the Reality of the Unknown
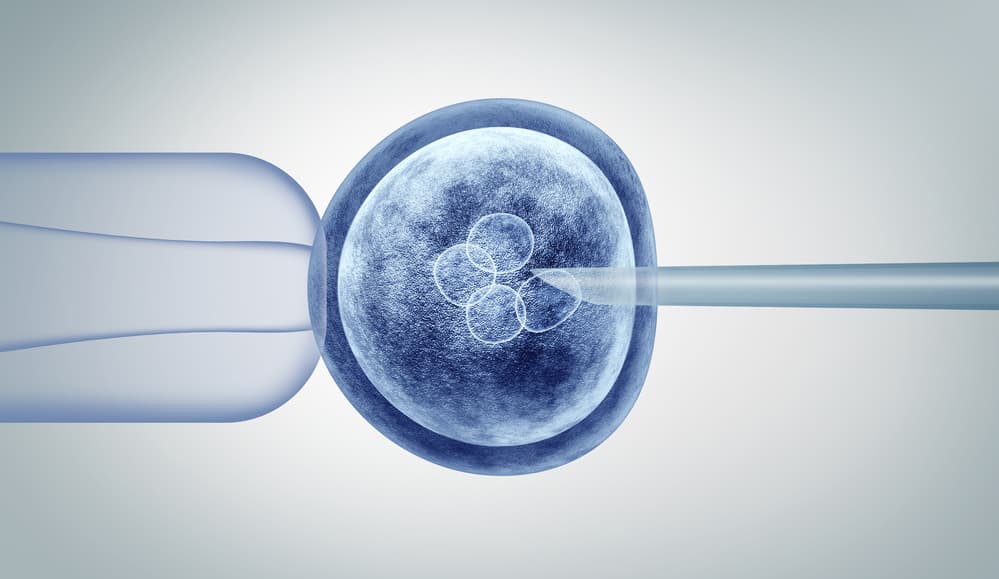
CRISPR/Cas9 and other gene editing tools allow scientists to make precise edits to DNA, replacing the faulty letter (one of the nitrogen bases in a DNA strand) with its healthy variant — which is all it would take to address genetic diseases where a single mutation to a DNA base leads to serious illness.
Many gene therapies for disorders, such as sickle-cell anemia and cystic fibrosis, are already undergoing clinical trials. A key difference in these studies is that they focus on editing the adult genome; any changes made will not pass into the germline and affect future generations. When working with germline cells, any change made, good or bad, will be passed to future generations and can have much farther-reaching consequences.
These gene-editing technologies are still in early development. Before applying what has been learned to heritable human genomes, scientists must demonstrate the ability to edit the exact location on a gene without introducing any unintended changes, and that these processes can be repeated consistently.
An Ongoing Scientific and Ethical Conversation
The Commission’s guidelines for clinical use of heritable human genome editing are intentionally strict. Though some are concerned that the guidance is too restrictive, many scientists fear that allowing wider adoption of heritable genome editing could eventually lead to enhanced embryos that are edited for desirable traits — the potential “designer babies” with improved athletic or intellectual performance.
In addition to the overall restriction to serious single-gene genetic diseases that will likely be inherited, the Commission also stated that there should be no other way of ensuring a couple can produce embryos without the disease-causing genetic variant. In vitro fertilization is one option that can allow doctors to screen embryos and only implant those without the genetic defect. Other technology not yet approved may offer alternatives to editing heritable genes, such as producing egg and sperm cells and growing embryos free of the genetic disease in the lab. In short, heritable gene editing should be the last remaining option for families, and only after it has been proven safe and effective.
By drafting the guidelines before broad segments of society approve of the ethics of editing heritable genes, the Commission has assumed societal acceptance will eventually proceed. This is the basis of some of the criticism of the published guidelines, which have not yet been adopted by any country or international authority. Critics state that establishing appropriate clinical use to determine the clinical route for safe administration of the technology prior to addressing the ethics is premature.
The Future of Heritable Human Genome Editing
As of now, more than 70 countries have banned the editing of heritable genes in humans. Opening a clinical route for heritable human genome editing requires more research, authoritative guidance, and ethical approval. As part of their guidelines, the Commission includes recommendations for scientific governance and oversight, so that each clinical use is evaluated independently and only approved when evidence has shown it is safe and effective. The Commission hopes to move toward this goal by advocating for both safety/efficacy and ethical conversations.
The International Commission on the Clinical Use of Human Germline Genome Editing submitted their draft guidelines to the World Health Organization (WHO) Expert Advisory Committee on Developing Global Standards for Governance and Oversight of Human Genome Editing. This WHO advisory is expected to publish their own official guidelines in the coming months — a preliminary draft is currently under review.
Since 1995, QPS has provided discovery, preclinical, and clinical drug development services. An award-winning leader focused on bioanalytics and clinical trials, QPS is known for proven quality standards, technical expertise, a flexible approach to research, client satisfaction, and turnkey laboratories and facilities. For more information, visit www.qps.com or email info@qps.com.




